Introduction about Barrier Nursing:
Barrier nursing is a largely archaic term for a set of
stringent infection control techniques used in nursing. The aim of barrier
nursing is to protect medical staff against infection by patients and also
protect patients with highly infectious Diseases from spreading their
pathogens to other non-infected people.
Barrier nursing was created as a means to maximize isolation
care. Since it is impossible to isolate a patient from society and medical
staff while still providing care, there are often compromises made when it
comes to treating infectious patients. Barrier nursing is a method to regulate
and minimize the number and severity of compromises being made in isolation
care, while also preventing the disease from spreading.
History & Usage of Barrier Nursing:
Barrier nursing started off as a term used by the Centre
for Disease Control (CDC) to describe early infection
control methods in the late 1800s. From the
mid-1900s to early 2000s, 15 new terms had emerged and were also being used to
describe infection control. The variety
of terms that described infection care led to a misunderstanding of practice
recommendations and eventual low adherence to isolation precautions; this
eventually forced the CDC to combine all 15 terms into one term called isolation. Nowadays barrier nursing is becoming a less
commonly used term and is not even recognized by most reputable databases or
online scientific journals. Yet when it is seldom used, it relates mostly to
circumstantial protocols for situations regarding isolation care. The lack of constant use of the term is why
there are no systematically reviewed articles on the topic and also why most of
the sources that include the topic are from the late 1900s.
Why do we need to Isolate/barrier nurse?
- To reduce the risk of spreading certain infections or antibiotic resistant germs to other patients and staff.
- To protect patients from infection if they have a weak immune system due to disease or taking certain drugs.
Barrier nursing is a largely archaic
term for a set of stringent infection control techniques used in nursing.
The aim of barrier nursing is to protect medical staff against infection by
patients and also protect patients with highly infectious Diseases from
spreading their pathogens to other non-infected people.
Some Important Techniques of Barrier Nursing:
Some Important Techniques of Barrier Nursing:
Hand Hygiene:
Hand washing also
known as Hand hygiene, is the act of cleaning one's hands to remove soil,
grease, Microorganisms, or other unwanted substances. Hand washing with soap –
often, and throughout the day – prevents the spread of many diseases.
Contact Precaution:
Contact precautions are
a series of procedures designed to minimize the transmission of infectious
organisms by direct or indirect contact with an infected patient or his
environment. Along with standard precautions, which assume all body fluids and
tissues are potentially infected with harmful microorganisms, contact
precautions require the use of protective equipment such as disposable gowns,
gloves, and masks when exposure to a patient's body fluids is anticipated.
Contact precautions are often used with patients who have wound or skin
infections.
Droplet Precaution:
Droplet precautions are
measures that have been developed to limit the airborne spread of
microorganisms in droplets that are larger than 5 microns in diameter (a micron
is 10−6 of a meter or one millionth of a meter). These droplets are typically
expelled into the air by coughing, sneezing, and even by talking.
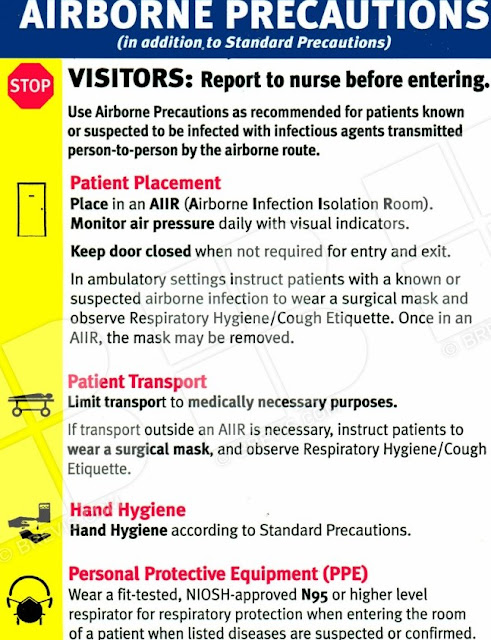
Airborne Precaution:
Airborne precautions
are procedures that are designed to reduce the chance that certain
disease-causing (pathogenic) microorganisms will be transmitted through the
air.
The precautions relate
to airborne, microbe-containing droplets that are less than five microns in
diameter (a micron is 10−6 meters). Such droplets can remain suspended in the
air for a long time and so can be transported a considerable distance (such as
from room to room) in even a gentle current of air. As well, particles of this
size can be inhaled deeply into the lung, where the chance of establishing an
infection can be increased.
Respiratory Hygiene:
Respiratory
Hygiene/Cough Etiquette in Healthcare Settings The concepts of respiratory
hygiene and cough etiquette involve using source control measures to prevent
patients with respiratory infections from transmitting their infection to
others.
To prevent the
transmission of all respiratory infections in healthcare settings, including
seasonal influenza, the CDC recommends implementing the following infection
control measures:
- Post Visual Alerts for patients and visitors
- Encourage Respiratory Hygiene/Cough Etiquette:
- Cover nose/mouth with a tissue coughing or sneezing
- When coughing, use a mask
- Use disposable tissues and discard after use
- Use hand hygiene after having contact with respiratory secretions
- Provide Respiratory Etiquette Materials for Patients and Visitors
- Offer Masks to Persons Who Are Coughing
- Separate Persons with Respiratory Symptoms.
- Advise Healthcare Personnel to Observe Droplet Precautions.
Safe Injection
practices:
Safe injection
practices include measures taken to perform injections in a manner that is safe
for patients and providers. Such measures are included in standard infection
prevention practices and apply to all patients in all healthcare settings.
Healthcare should not provide a pathway for transmission of bloodborne viruses
to patients or providers.
Use of mask for
insertion of catheters and epidural or spinal catheter.
Meaning of Reverse Barrier Nursing:
Reverse Barrier Nursing is concentrated on protecting vulnerable
patients, such as those with weakened immune system, against infection carried
or transmitted via medical staff.
Such is given in neutropenic patients, post transplant
patients, premature infants etc. This include:
Wearing PPEs by the staff to prevent contact, airborne and
droplet infection to the patient considering all staff as a potential carrier
of infections.
- Isolation in positive Pressure isolation rooms
- Use of sterile items or Disposable items
- Neutropenic food (Microwaved after cooking)
- Hygienic environment
- Minimum Traffic in the room
- Patient to be minimum transposed and use of PPEs by the patient
to prevent catching of infection
Written by:
Dr. Praveen Bajpai
Director of Ingenious Healthcare Consultants Pvt. Ltd.
Founder of Skill Sathi
MBA in Hospital administration, PG Diploma in Quality Accreditation, PG Diploma in Medico Legal System, M. Phil in Hospital Mgmt. from BITS Pilani, P.hD in Management, Certified NABH Auditor, Certified NABL Auditor, Certified Auditor for Clinical Audits, Green Belt in Six Sigma, Certified in Hospital Infection Control Practices, Certified trainer for International Patient Safety Goals, Certified Auditor for JCI 7th Edition Standards
www.skillsathi.in












Comments
Post a Comment